In 2008, my son Michael was diagnosed with a urea cycle disorder called Argininosuccinic Aciduria (ASA) at just three days old. ASA is rare genetic disorder characterized by deficiency in an enzyme called argininosuccinate lyase (ASL). ASL is one of six enzymes that facilitate the breakdown and removal of nitrogen from the body – a process known as the urea cycle. A lack of ASL causes an accumulation of nitrogen in the form of ammonia. In the short term, this excessive ammonia can cause seizures, respiratory abnormalities, fluid in the brain and an enlarged liver. In situations where the ammonia is elevated for a prolonged time, symptoms can progress to coma, neurological deficits, developmental delays, intellectual disabilities and even death. The treatment for urea cycle disorders are dietary restrictions, enzyme supplementation and ammonia scavenger medication. Living with ASA or any of these disorders is extremely challenging. A diet needs to be strictly followed with all food counted, weighed and documented in a log. Protein metabolism produces the most ammonia, and therefore protein needs to be restricted. Protein is in everything! Kids like Michael have to avoid foods such as meat, chicken, fish, dairy, eggs, nuts and pasta due to their high protein content. Eating too much protein could quickly send him into crisis and require emergency medical attention.
Michael was not our family’s first-born child. In 2004, we had a daughter named Mia. With this disorder being a recessive trait, Mia may be a carrier of ASA, though she does not have an active case. But when Michael was three years old, our family decided to have a third child. After consulting with Michael’s metabolic physician and completing genetic testing, we were told that it would be extremely unlikely for a third child to have the same disorder. The chances of having back-to-back births resulting in multiple children with ASA are very low. In 2011, we became pregnant and were so excited to announce the news. A few months later, we tested our unborn little girl for the same Urea Cycle disorder as her brother. And just before Christmas, we got the call that nobody thought would come: we got confirmation from the genetic councilor that our unborn daughter Marisa did, in fact, have ASA. It was unthinkable that with only about 100 cases in the U.S., we were going to have two kids with a life-changing disease. The only silver lining was that Michael was always going to be different, and he would now have Marisa to navigate this journey with.
Living with a urea cycle disorder is mentally overwhelming, physically exhausting and financially devastating. The everyday struggle of giving your kids just enough food so as not to harm them but still provide them with enough nutrition to grow and develop is difficult to handle. The stress of not knowing if your children were going to wake up in the morning because of what they ate that day was something we dealt with every single night. Food is very social, but for a person living with a UCD, it is a life or death situation. To compound the situation, there was no way to test ammonia at home. So as parents, trying as hard as possible to manage the food log and the daily intake expectations, we could not see trouble until the symptoms were visible and obvious.
Michael and Marisa needed accommodations everywhere they go. At birthday parties, they could not have pizza, cake or ice cream, so they would eat French fries. Family gatherings and holidays would have to include low-protein food options. On Thanksgiving or Christmas, while everyone was eating turkey, prime rib, ham, or stuffing, Michael and Marisa would be eating vegetables or guacamole and chips.
Innovation and research has been crucial to Michael and Marisa’s survival. Their treatment plan is the result of provider collaboration. Metabolic geneticists from all over the world are constantly sharing new discoveries, experiences and outcomes. There are organizations such as the National Urea Cycle Disorder Foundation with the mission to drive research for kids suffering from these diseases. Another impactful result of innovation and research are ammonia scavenger medications. During Michael’s first couple of years of taking medication, there were only a couple of options available, and both were unpleasant experiences coupled with many side effects. Thankfully, a breakthrough was made and a new medication was developed. Both Michael and Marisa were part of a study that brought a trial medication to market, which was more concentrated and resulted in a smaller, tasteless and odorless dose with the same effectiveness.
Most recently, Michael and Marisa benefited from liver transplant advancements. In October 2014, they were both listed for a liver transplant at the Children’s Hospital of Pittsburgh. We fully understood the risk of major surgery and the reality of potentially trading one set of problems for another. But due to the life-threatening challenges of living with a UCD and a treatment that most providers would call sub-optimal, we decided a transplant would be the best long-term plan for our children. We felt the advancement in liver transplant surgery would provide a better life for the kids. They would still need to take medication daily, but the diet restrictions and fear of hyperammonia or a medical crisis would be eliminated.
On January 3, 2015, Michael received his new liver, and on July 27,2015, Marisa had her surgery. Today, they are healthy and happy kids living their best lives! There is a continued need for research and innovation for kids living with the horrific disease.
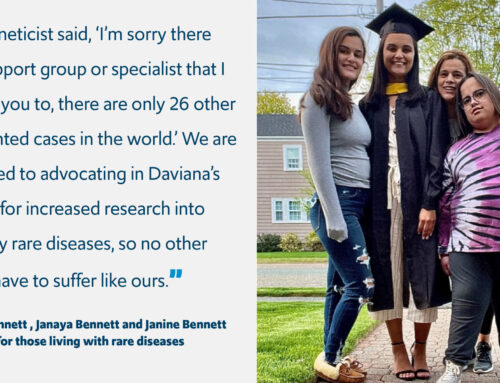
Michael and Marisa Vestal
Living with Argininosuccinic Aciduria (ASA)